- +1 800 433 4609
- |
- Request Info
PWV Analysis Parameters
Ejection Elasticity Index (EEI)
EEl is an indicator of large artery stiffness and left ventricle ejection power.
Decreased value (<0.3): Indicates potential ejection insufficiency of left ventricle, atherosclerosis, endothelial damage. Possible causes include hypertension, -Creactive protein, homocysteine, high cholesterol diabetes, or obesity.
Increased value (>0.7): Indicates potential for increased ejection power of left ventricle. Possible causes include anxiety, pharmaceutical and/or nutraceutical reaction.
Dicrotic Dilation Index (DDI)
DDI is an indicator of small artery compliance, tension and stiffness.
Decreased value (<0.3): Indicates small artery constriction due to arteriosclerosis, atherosclerosis/endothelial damage. Possible causes include hypertension, C-reactive protein, homocysteine, or high cholesterol.
Increased value (>0.7): Indicates vasodilation. Possible causes include anxiety, pharmaceutical and/or nutraceutical reaction.
Dicrotic Elasticity Index (DEI)
DEl is an indicator of arterial elasticity and blood flow through peripheral arteries (capillaries).
Decreased value (<0.3): Indicates potential loss of arterial elasticity. Possible causes include arteriosclerosis, atherosclerosis/peripheral vascular disease/inflammation.
Increased value (>0.7): Indicates vasodilation. Possible causes include anxiety, pharmaceutical and/or nutraceutical reaction.
Augmentation Index (AI)
Augmentation Index measures arterial stiffness. Arteries stiffen for a number of reasons including age, high cholesterol, smoking and diabetes. The stiffer and more hardened an artery is, the more difficult it is for blood to flow through the body. To compensate for inefficient blood flow, the heart must work harder.
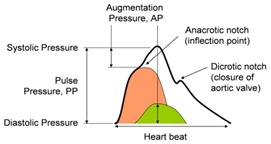
Augmentation index is calculated using pulse wave velocity. A ratio is calculated from the blood pressure waveform derived from PWV analysis. AI is widely used as a measure of the augmentation of central aortic pressure by a reflected pulse wave (shown in green in the graph).
Why does Augmentation Index matter?
Augmentation index is an important biomarker of arterial status. AI is useful for the following:
• Predict major cardiovascular events (higher augmentation index is associated with target organ damage).
• Analyze the varying effects of different vasoactive medications (cuff blood pressure and PWV do not show this)
Calculating Augmentation Index
Central augmentation index (cAI) is defined for a central pressure waveform as the ratio of augmentation pressure (AP) to pulse pressure (PP):
cAI = AP / PP
The wave shape is dependent upon where the pressure waveform is taken from (i.e. upper arm or wrist). In some instances, late systolic pressure may be higher than early systolic pressure. Meanwhile, in other instances, no pressure augmentation is visible (late systolic pressure is lower than early systolic pressure). See the figure below:
Peripheral augmentation index (pAI) is defined as the ratio of late systolic pressure (P2) to early systolic pressure (P1):
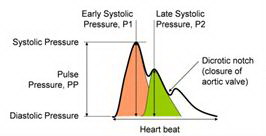
pAI = P2 / P1
Frequently Asked Questions – Augmentation Index
1. How does PWV Analysis measure augmentation index?
AI is a ratio determined using the peripheral augmentation index formula (i.e. pAI = P2 / P1).
2. How accurate is the PWV Analysis measurement?
The maximum potential for error is just 4% of the typical measurement range. This level of accuracy has been checked against expert analysis of 50 measurements taken from a cross-sectional clinical study.
3. Does PWV Analysis correct for heart rate when calculating augmentation index?
It has been suggested that higher heart rates lower the central augmentation index since decreases in heart relate to increases in AI. However, since the relationship between heart rate and peripheral augmentation index has not been formally the PWV Analysis does not account for heart rate.
A white paper detailing an advanced PWV Analysis of pressure wave components is available to provide direct insight into these effects.
4. Is augmentation index related to:
a. Age?
Yes. Both AI and central blood pressure increase with age.
b. Gender?
Yes. On average, women have a higher augmentation index than men.
c. Central blood pressure?
Yes. There is a statistical relationship between augmentation index and central blood pressure.
d. Height?
Possibly. There is some evidence to suggest that in shorter individuals, a shortened return time for reflected waves leads to an increase in central pressure augmentation.
e. Cholesterol?
Yes. Central augmentation index positively correlates to cholesterol levels even though cholesterol may or may not relate to functional measures of cardiovascular health.
f. Body mass index (BMI)?
No. However, studies show that high body fat content - but not BMI - is strongly associated with increased large arterial stiffness.
5. Does brachial artery, arm or cuff variation affect the measurement?
As augmentation index is a ratio, variations in the arm, cuff or brachial artery produce minimal effects in the readings. Further, the brachial artery is less affected by disease than other major arteries so therefore it upholds a high level for measurement.
Augmentation Index Summary
The Arterial Vascular Assessment determines parameters such as Augmentation Index, Augmentation Index (AIx) and Pulse Wave Velocity (PWV) using an additional, highly sensitive vibration sensor. Oscillations are registered by a blood pressure cuff with suprasystolic pressure. These measures reflect vascular rigidity and aging. The resultant AIx data may be used for early prediction of cardiovascular events or screening of endothelial and vascular dysfunction.
Augmentation, as a function of pulse wave reflection, is highly dependent on pulse wave velocity. In turn, pulse wave velocity is dependent on vessel elasticity. The augmentation index reflects the ratio of augmentation to pulse pressure.
Augmentation index classification
• AI < -30 % optimal
• -30% < AI < -10% normal
• -10% < AI < +10% elevated
• AI > +10 % abnormal
Reflection Index (RI)
The reflection index (RI) indicates the relative height of the diastolic peak. This value is expressed as a percentage of the total amplitude of the DVP waveform.
Essentially, RI is a calculation of the percentage of pressure wave (PW) reflected back from. This same idea is used to understand ripples in a puddle of water. If a pebble is thrown into a puddle, the energy from that pebble will cause waves to ripple out to the edges. As the ripples reach the edge, they will reflect back toward the center but with less energy on their return. Applying this principle to blood flow, RI measures the reflection back from where the small artery narrows. This value correlates to the condition of the small arteries.
Anything that influences vascular tone or the condition of the endothelium (i.e. the arterial lining) affects the RI. The more stressed the endothelium, the less energy will be absolved and the higher the RI value will be. Even caffeine and exercise may influence the RI reading.
Applications of Reflection Index
1. Vasoactive drug assessment:
Vasoactive drugs effectively reduce arterial tone thereby influencing the pressure wave reflection. The PWV System is easily incorporated into a drug management program to measure RI in a noninvasive manner.
2. Endothelial function testing:
Endothelial issues are one of the primary precursors to developing vascular diseases. Measuring the change in wave reflection in response to endothelium-dependent vasodilator drug (salbutamol or albuterol) facilitates the assessment of endothelial function. The PWV System provides the RI measure to be used for pulse contour analysis and ultimately test for endothelial issues.
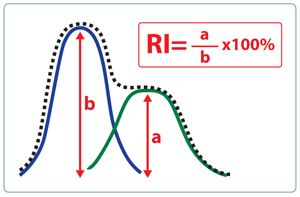
The RI test illustrates the percentage of reflected pressure wave. The average RI reading is between 60-90% however lower figures are not uncommon.
Stiffens Index (SI)
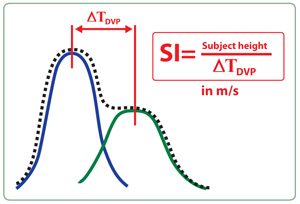
Increasing evidence suggests that arterial stiffness may be the primary indicator of future cardiovascular events. Stiffness influences the speed by which pulse is propagated through the body. The timing of the reflected wave (diastolic component) relative to the direct wave (systolic component) is directly dependent on the condition of the arteries.
The stiffer the artery, the quicker the reflected wave returns to the heart versus with more compliant/elastic arteries. The PWV System provides a Peak-to-Peak Time (PPT) measure to indicate the estimated propagation time of a reflected wave. If the arterial tree length is proportionate to the patient’s height, this stiffness index (SI) will be derived by dividing the height by the peak to peak time.
The reading is a snapshot of one moment in time and not an overview of the cardiovascular system. A number of factors influence the cardiovascular system including stress and diet. As such, it is recommended that regular periodic testing is administered over a time period to glean accurate results. See figure below.
PW = Pulse wave. Each heart beat produces a wave of pressure referred to as a pulse wave (PW).
PWV = Pulse wave velocity. Describes the speed at which the pulse wave (PW) travels. This value is measured in meters per second (m/s) and is dependent on the condition of the arteries. Stiffness speeds up the PWV while a flexible, compliant artery slows it.
Understanding (SI) results:
A good result is when the reading is less than two thirds the height of the green section in the above bar graph. If the reading is towards the top end of the green bar or nearing the red region, this could indicate some risk. Lifestyle changes such as proper diet, increased physical exercise, proper hydration, stress management, quitting smoking and supplements may be the solution.
Acceleration Plethysmogram (APG)
The second derivative of PTG/PWV is an effective method of evaluation vascular age.
Element of APG
b/a : Smaller peak with age. LV ejection and compliance of large artery.
c/a : Lower with age.
d/a : Larger peak with age. Contraction and tension of small artery.
e/a : Lower with age.
