- +1 800 433 4609
- |
- Request Info
Pulse Wave Velocity Analysis (PWV)
The Pulse Wave Velocity assessment is performed using an infrared finger clip probe that measures blood volume changes. The amount of light absorbed is directly proportionate to the volume of blood in the finger. When the heart contracts, it produces a direct wave that travels down to the finger. This wave is reflected in the lower body as well as down to the finger. It is this combination of the direct wave and reflected wave that is measured and recorded by the finger probe.
The pulse wave is a physiological phenomenon, observable and measurable in the arterial system during blood circulation. During one heart systole a certain blood volume is expelled. This propagates through the arteries due to the reciprocal transformation between kinetic energy of a segment of the expelled blood volume and the potential energy of a stretched segment of the resilient vascular wall. We can observe the changes in pressure, blood flow, velocity and profile throughout the whole pulse wave. It can be used for classification of the artery elasticity.
Pulse wave velocity analysis is a classic index of aortic stiffness and is a predictor of cardiovascular mortality in hypertensive cases. Since aortic pulse wave velocity is dominantly influenced by age, this finding may be of major importance for the evaluation of cardiovascular risk in the elderly.
Aortic PWV nowadays is considered as a marker of CV risk independently of blood pressure level, but in conjunction with heart rate. Since PWV is increased particularly in the elderly, this analysis may be considered as important for geriatric populations.
S (Starting point)
Starting point of arterial pulse-wave. Aortic valve opens and the blood of the left ventricle is discharged.
P (Percussion wave)
Wave caused from LV ejection that increase the arterial wall linearly.
T (Tidal wave)
Reflected wave from the small artery.
C (Incisura)
End-point of systolic phase, then aortic valve is closed.
D (Dicrotic wave)
Reflective oscillatory wave occurred from the blood crash into aortic valve by blood pressure of aorta.
Early detection of
1. Hypertension
2. Arteriosclerosis (hardening of the arteries)
3. Blood circulation status
4. The relative age (biological age) of blood vessels
5. Disturbances in the smaller blood vessels not found when measuring you blood pressure with a cuff
For Early assessment of
1. Cardiovascular health
2. Management of disease progression,
3. Monitoring the effects of medication, therapies, lifestyle changes and dietary habits
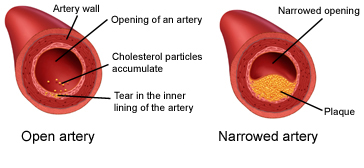
PWV Analysis -Arterial stiffness indexes (EEI, DDI and DEI) can additionally suggest to healthcare professional to begin appropriate treatment long before the symptoms or clinical signs appear. Age and systolic pressure strongly correlate with PWV. In fact, the most important factor contributing to increase in PWV is age because of increased arterial stiffness caused by medial calcification and loss of elasticity. Some studies suggest that the increase in PWV could be an early indicator of atherosclerosis development (as diabetes); other studies show no significant difference in PWV with age in subjects predisposed to a high risk of atherosclerosis, such as familial hypercholesterolemia. However, there has been a qualitative association between the process of atherosclerosis and arterial rigidity; PWV studies indicate that hypertension contributes more than atherosclerosis to increased arterial stiffening with age.
Large artery damage is a major contributing factor to the elevated cardiovascular morbidity and mortality observed in cardiovascular risk factors such as hypertension. Reduced arterial distensibility contributes to a disproportionate increase in systolic pressure and an increase in arterial pulsatility, which has been shown to be associated with an increase in cardiovascular morbidity and mortality. Pulse wave analysis provides information on stiffness and distensibility of an artery. The measurement of pulse wave velocity is useful in the study of the effects of aging, vascular diseases, vaso-dilating and vaso-constricting agents on arteries.
Reduced arterial compliance in non-occluded arteries has been demonstrated in patients with coronary artery disease and in patients with diabetes mellitus. Atherosclerosis causes the arterial wall to become thicker and harder and narrows the arterial lumen The increased inflexibility of the arterial wall serves to increase PWV, because the energy of the blood pressure pulse cannot be stored in an inflexible wall.
The condition of the major arteries is the key to better prevention and diagnosis of cardio-vascular related illness. In particular, the stiffness of the major arteries is a strong indication of potential health problems including, heart attacks, heart failure, diabetes, and renal complications. While blood pressure is a useful first-level indicator of hypertension, it doesn't give the full picture. During the test, the baroreflex-induced pulse pressure changes the elastic properties of the arterial wall and induces its movement. The effects of the baroreflex can be measured by measuring the movement of the arterial wall.
VitalScan Pulse Wave Velocity measurement a part of the HRV analysis acts as a supplemental convenient way to quantify stiffness of the major arteries. VitalScan - Pulse Wave Analysis - Four minute procedure during Resting, is non-invasive, cost effective supplemental indicative measurement of the relative health of major arteries, but also to monitor the effects of any ongoing therapy, treatment or dietary changes.
Screening risk factors by early detection of abnormal arterial-wall function
* Identifying the arteriosclerosis and arterial aging.
* Monitoring the effect of treatments for patients with hypertension and other cardiovascular disease.
* Evaluating the efficacy of prescribed lifestyle modification and medications.
Pulse Wave Velocity Results
Ejection Elasticity Index - Capacitative Compliance
Indicates Left Ventricular thickness, Ejection level and Elasticity of Large Arteries.
Normal = 0.3 to 0.7
Decreased value = < 0.3 = possible left ventricular ejection insufficiency / Atherosclerosis; possible hypercholesterolemia
Increased value = > 0.7 = possible increased left ventricular ejection power / anxiety
Dicrotic Dilation Index - Oscillatory Compliance
Indicates Contractility, Compliance and Stiffness in Small Arteries.
Normal = 0.3 to 0.7
Decreased value = < 0.3 = possible hypertension and/or arterial sclerosis (arterial stiffness); constriction in small arteries.
Increased value = > 0.7 = dilation of artery (possible due to acute anxiety)
Dicrotic Elasticity Index
Indicates Reflection of Peripheral Arteries/Arterial Elasticity - Blood flow in the venous system.
Normal = 0.3 - 0.7
Decreased value < 0.3 = possible decreased vessel elasticity/arteriosclerosis in the peripheral portion of the arteries
Increased value > 0.7 = dilation of arteriole
Aortic Stiffness
Higher Pulse Wave Velocity in an aging stiffer Aorta causes The Reflected Wave to return to the heart early, arriving in mid Systole.
This independently increases the risk of THREE major cardiovascular outcomes.
Increased Central Pulse Pressure
• Central systolic pressure is increased.
• Increased stress on cerebral blood vessels increases stroke risk.
• NOTE: This change in central systolic pressure can occur without any changes occurring in peripheral cuff systolic pressure.
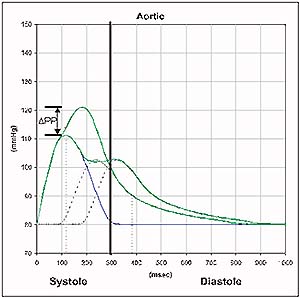
Increase Left Ventricular Load (LV Load)
• Left ventricular load (LV load) is increased.
• Increase in LV load accelerates increase in LV mass and increases LV hypertrophy.
• The area under the pressure-time curve during systole is by definition LV load.
• This increase in LV load is shown by the black arrowed region.
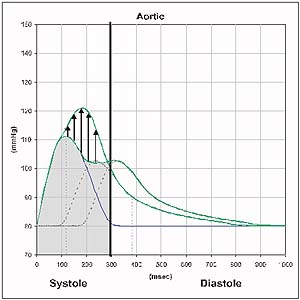
Decreased Coronary Artery Perfusion Pressure in Diastole
• The pressure that is perfusing the coronary arteries during the critical diastole period is reduced.
• This increases the risk of myocardial ischemias.
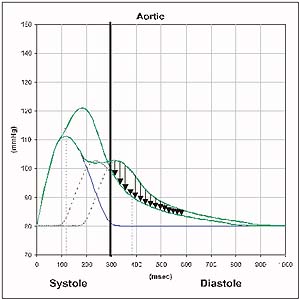
Aortic stiffness has been well validated as an excellent predictor of cardiovascular health and illness.
